| Preface
In 1997, WHO listed “obesity” as the third chronic killer after smoking and AIDS. Modern people are afraid of “obesity” and become particularly sensitive to the increase of body weight and change of figure. It is especially so in females, and for the purpose of keeping fit, they try by every possible means to “reduce fat”. But what is the result? Most of them ended in disappointment. The chief reason is that the real cause of producing obesity and the correct method of treating it are not found out. The current “obesity epidemic” is spreading over the whole world “Obesity” is an epidemic, this is an undeniable fact, and in many places, numerous statistical data prove this tendency. In the middle of May this year, the annual meeting of WHO issued its newest research material: “Obesity is not only an ‘epidemic’ of developed countries, but also a disease with the acknowledged characteristics of “wealthy society”, spreading to the developing countries. It is estimated that there are about 300 million people suffering from obesity and about 750 million are over weight. In some countries, 30% of the children belong to the fat group and about 22 million children under five years old are overweight or too fat. For example, in Africa, to our surprise, the number of fat children is four times of the undernourished…..”. Statistics in America indicated that from the sixth decade onwards, obesity patients increased by more than a double. The “abnormally fat” population increased from 13% to 22.5% in 1994, and in 1999 to 27%, while the age of the patients becoming younger and younger. In America, there are about 100 million people (97 million adults) over weight or abnormally fat, occupying 55% of the total population. The investigation of North Carolina University in America showed that more than 1/4 of the American population suffered from obesity (male 20%, female 28%). Countries of European Union have 1/3 of their population overweight and there is one obese person in every ten.
From these scattered and incomplete statistical materials, we can still see that “obesity” is really a problem of the whole world. Specialists consider that morbid fatness is an epidemic in the field of public health and the number of victims is up rising. In fact, one would be reluctant to accept that he is fat. Besides, fatness also affects seriously human health. It is unsatisfactory to explain by saying that obesity is simply due to “lack of physical exercise” and to “over nutrition” in modern life or that “the conventional diet habit tends to be substituted by taking high fat instant food or the daily life limited in a small area with insufficient physical exercise”. |
|
|
Differentiate “simply obesity” and “secondary obesity” Hepatogenic secondary “obesity” is due to infection by “hepatophilic virus”. We can not consider obesity as “disease of the rich”. When the calories taken are more than those consumed, the remaining nutritional materials are transformed into fat, which is stored in various tissues and also under the skin and then “obesity” is formed. From the medical point of view, obesity includes “simple obesity” and “secondary obesity”. “Simple obesity” is obesity caused by simple over nutrition. In this kind of obesity, the distribution of fat is even without showing any significant anatomic or formational changes in nervous or endocrine system. Therefore, individuals with mild or moderate obesity usually have their skin delicate and full of luster, abdominal circumference larger but still preserving a loin curvature, umbilicus deeply mined, fat pads protruding around the central umbilicus and curving depression seen at the outer side of sheath of rectus abdominal muscle, causing the fat pad to be more prominent. These individuals have full breasts and buttocks, normal mental condition and good health. The correct method for them to reduce fat is to control food intake adequately, reduce high lipid and glucose diet, do some physical work or exercise and cut down extra-dietary food and calorie intake. Fat reduction method is only effective for simple obesity. “Secondary obesity” is basically different from simple obesity. The main cause, in most patients, is disease in the body leading to accumulation of fat. Secondary obesity is often associated with some other diseases; it may be secondary to certain primary disease in the body and may also be the result of development of certain disease, e.g. hepatogenic obesity (肝源性肥胖), diencephalon obesity (間腦性肥胖), pituitary obesity (垂體性肥胖), (induced by various encephalitis, meningitis, brain injury, brain tumors causing damage to diencephalon and pituitary) sex gland dysfunctional obesity, adrenocortical hyperfunction obesity (腎上腺皮質機能亢進性肥胖), hypothyroidism obesity (甲狀腺機能過低性肥胖), insulin obesity or improper use of drugs (such as abuse of adrenocortical hormones leading to adverse effects like full moon face, sodium retention or prolonged use of sex hormones). The above endocrine disorders all can produce secondary obesity.
|
|
| Mechanism of producing hepatogenic secondary obesity by hepatophilic virus infection
Recent clinical observation reveals that increasing incidence of secondary obesity is found to occur in the acute hepatitis convalescence stage and during chronic active hepatitis. Some cases can be confirmed as “fatty liver” and some are in the stage of “nutritional disorder” produced by metabolic disturbances after infection by “hepatophilic virus” and by prolonged suffering from chronic hepatitis resulting in diseases of various systems. Abnormality of liver function can also cause endocrine disorders which may produce “hepatogenic secondary obesity”. When the human body is infected by hepatophilic virus, the immunologic reaction can cause the liver to develop acute or chronic inflammation. We have mentioned that “hepatophilic virus disease” means that the patient has abnormal margin of hepatic dullness, clinical persistent & repeated, alternating and multiple systemic symptoms of chronic hepatitis and various diseases and complications induced by acute or chronic liver function damage. The disease includes defect in absorption of nutritional material, leading to malnutrition, prolonged anemia, hypoproteinemia (低旦白血症), bleeding from abnormality of clotting mechanism and all these conditions can cause ischemia of pituitary (垂體缺血) and subsequent endocrine disorder. Protective function of the body can lead to over production and retention of adipose tissue which forms hepatic edema, fatty liver and secondary obesity. So, it is doubtless that fatty liver, hepatogenic secondary obesity and hepatic edema are common complications and sequalae of hepatophilic virus disease. In addition, most of the patients with secondary obesity have still a dysfunction liver when first seen by physician. If there is no provision of effective systemic TCM therapy, the chronic hepatitis may persist and gradually complications of heart, blood vessels, apoplexy and diabetes may appear. Obesity can also induce respiratory diseases, muscular and dermal problems, infertility, hypertension and hormone related cancer complications, leading to dysfunction of heart, lung and kidney. Although “abnormal obesity” can induce many complications, but these complications together with “abnormal obesity” are in fact the result of the persistence of chronic “liver disease”.
|
|
|
“Epidemic”— characteristics of hepatogenic secondary obesity
The above mentioned patients may not easily obtain fat reducing results through ordinary fat reducing measures. But the application of “effective systemic TCM therapy” can give clinical cure in chronic hepatitis. Further more, it may be able to correct hepatic edema and hepatic obesity, terminate the progression of chronic hepatitis and make the liver function normal and can eventually avoid the development of complications of obesity.
|
|
| Modern obesity epidemic spreading all over the world
Liver disease is regarded as an infections disease and the fact that induces hepatogenic secondary obesity and that the saying “hepatogenic secondary obesity is epidemic” is not at all irrational. Patients with obesity have increased rapidly in recent years. It is closely related to the recent development of science, frequent communications among people in all corners of the world and the increased chance of hepatophilic virus infection. Data from many places indicate that in the world patients with obesity are increasing every year and their age are becoming younger. If these cases are “hepatogenic secondary obesity”, it indicates that “hepatophilic virus” is silently disseminating in the human community with a high speed. Nowadays, people gradually understand that we must not neglect the harmful effects of “hepatophilic virus” upon human health and the above statement about the cause of hepatogenic edema (or secondary obesity) by chronic hepatitis is an undoubted evidence. The only method to cope with this situation is to take preventive measures at the very beginning, that is to say, detect and treat “chronic hepatophilic virus disease” at an early stage. This is the best way to reduce fat and prevent secondary obesity. It we still use the erroneous old method of reduction of food in take, food preference, or increase exercise blindly, or improper administration of fat reducing drugs, the result will be squander of money or even serious impairment of health.
|
|
| Information about obesity
According to standard body weight, over 10% of standard body weight is regarded as over weight while over 20% of standard body weight is regarded as obesity.
The body mass is measured by the Body Mass Index (“BMI”), i.e. body weight (kg) in proportion to body height (M2): Body Mass Index (BMI) = Body weight (kg)/body height 2 (M2)
Chinese adult standard of obesity Recently, a report was given by Prof. Chou Bei Fan of Epidemic Disease Research Institute, Fou Wai Cardiovascular Disease Hospital, Chinese Academy of Medical Sciences, stated that the Chinese obesity working team, according to the data collected during the ninth decade of 20th century, made an analysis which first suggested a standard of obesity suitable for Chinese adults:
|
|
|
Introduction of cases Case 1 Shu (code number 2612), female, age 32 years. Her first visit was in August 2001, with the complaint of suffering from hemorrhoids two years ago. From time to time, she experienced poor appetite, abdominal pain and distention, constipation, hematochezia and she had an increase of 10 lbs of body weight. She was hospitalized once because of insomnia, palpitation, dim eyesight and vertigo. Her height was 1.57 meter, weight 65 kg, BMI 25.39. Physical examination: marked swelling of lip mucosa, hepatomegaly of 1.5 cm with percussion tenderness, (+) pitting edema over pretibial region. The TCM diagnosis was wetness-heat vaporization, blockage of channels and blood stasis and secondary obesity. After taking 3 parcels of TCM drugs, the liver returned to normal. Through systemic TCM therapy, the body weight reduced to 50 kg, BMI 18.86. She lost about 33 lbs and the abdominal circumference was 73 cm, buttocks circumference reduced from 40 inches to 34 inches. She was now receiving premenstrual TCM therapy. |
|
| By WONG Kwok Hung
Published on 25th July 2002 Translated by Professor Zheng in January 2005 |
All posts by mapp_user
Hepatogenic “edema” is not “obesity” (One of the common syndromes of “deficiency of blood and weakness of qi “
| Preface
Not a few people think themselves “obese”, but they do not know in fact it is hepatic edema. Because hepatic edema can cause progressive increase of body weight and body figure, so, often times it is erroneously considered as “obesity”. Actually, many people confuse hepatic edema with “obesity”, and many are misled to adopt incorrect therapeutic measures, for example, abatement of weight can contrarily aggravate edema or even cause “anorexia” which may seriously affect one’s health.
Edema is essentially different from simple obesity. From the TCM point of view the concept that “nine out of ten obese individuals belong to the category of wetness” is extremely correct. Edema is also called water puffiness, it is due to excessive fluid retained in the skin and subcutaneous tissues (including spaces in extra-vascular tissues); weighing the body at regular intervals let one know the degree of edema.
Usually, the appearance of edema of face and mild edema of lower limbs indicates that the body weight has already increased 5%. If edema in these places is marked and pitting edema is present (use the finger to press on the skin over tibial region with persistent mild force, and a pit can be seen when the finger is released) and if the trunk is also edematous, the body weight may have increased about 10%. What are the causes of edema? There are many causes, for example, nutritional, endocrine disease, water and electrolyte imbalance, drug allergy or intoxication. According to the chief causes, one may differentiate, clinically, cardiac edema, hepatic edema, renal edema or nutritional edema. The following is concerned with hepatic edema, our understanding about which offers to the public for the purpose of reference.
|
| Hepatic edema
Hepatic edema is very common but, at the same time, easily neglected by patients and physicians. According to clinical observation, the causes of hepatic edema are many and complicated. The main reason is that in patients with liver disease, the concentration of retained “antigen-antibody compound” in the body increases as time passes by, leading to the accumulation of inflammatory exudates in tissue spaces and subsequently, formation of hepatic edema.
It is not difficult to justify oneself the existence of hepatic edema or not. The following questions may be asked :
The answers to the above questions can tell you whether you have hepatic edema or not. Some people consider themselves “obese” but in fact they are having hepatic edema. Our research centre received 2883 patients with abnormal margin of hepatic dullness in Hong Kong. Among these cases, 952 had various degrees of hepatic edema, occupying 33% (proportion of male to female is 238 : 75) male 23%, female 38.5%. From the statistics, it can be seen that in Hong Kong, where the incidence of liver disease is high, hepatic edema is extremely common. In all of the cases, about 1/3 have various degrees of edema clinically, and in females with abnormal margin of hepatic dullness, about 40% have hepatic edema, significantly higher than the male 23.19%. This is related to the high proportion of deficiency of both qi and blood form in female chronic hepatitis patients and it indicates that hepatic edema is closely related to deficiency of qi and blood and also to anemia.
In the above paragraphs, we have mentioned that hepatophilic virus disease is a disease in which the patient presents abnormality of hepatic dullness, clinical chronic hepatitis conditions showing obstinate, repeated, alternating and multiple systemic symptoms and various diseases induced by acute and chronic damage of liver function. Therefore, it also includes hepatophilic virus infection induced hepatic edema which is caused by “deficiency of qi and weakness of blood”, dysfunction of nutrition and absorption, malnutrition, anemia, hypo-protinemia, endocrine disorders, vitamin deficiency (such as wet beriberi caused by deficiency of vitamin B1).
|
| Severe cases may lead to cirrhosis or carcinoma of liver
In fact, hepatogenic edema, hepatic secondary obesity, and fatty liver all are complications and sequelae of hepatophilic virus disease. It is when the course of chronic hepatitis has entered a comparatively serious stage that hepatic edema would appear clinically. If the condition is not treated by systemic TCM therapy, the degree of edema deepens day by day and it may induce cirrhotic ascites, dysfunction of the heart and lungs or even carcinoma of liver; the latter would often be discovered too late. The former condition is difficult to treat but is still reversible. So, hepatogenic edema is not “obesity” and one should not go after reducing fat blindly.
|
| Abuse of fat reducing drugs damages liver function
From the viewpoint of TCM, “nine out of ten obese individuals suffer from wetness” and this concept is very correct. There is a basic difference between hepatic edema and simple obesity; one must correctly differentiate what is edema and what is obesity. One should not think oneself obese on sheer assumption and take fat reducing measures blindly. If patients with hepatic edema reduce food intake, limit protein ingestion and increase exercise amount which leads to consumption of body energy, or, for the purpose of reducing fat, even take drugs that damage the liver, the hepatic function would be markedly impaired and the liver disease greatly exacerbated.
|
| Drugs should aim at cause of edema
Hepatic edema is not simple obesity caused by over nutrition; it cannot be cured by reducing fat. The edema can be eliminated only by treating the liver disease, that is, by the use of effective TCM therapy. The extended margin of liver dullness can return to normal after several days of treatment and the continuation of therapy can further induce significant regression of edema. We therefore suggest that before taking fat reduction measures, one must make clear that the edema is not caused by liver disease. If hepatophilic virus disease can be detected early and is known to have developed hepatic edema and secondary obesity, TCM and WM therapy should be undertaken in time. In this way, the patient can avoid prolonged suffering from various systemic symptoms of chronic hepatitis and can stop the persistence of edema and secondary obesity and can also keep the body in a healthy condition and prevent progression of the liver disease into cirrhosis or carcinoma.
|
|
Cause of hepatic edema
Chromic virus hepatitis produces hepatic edema caused by attack of infections hepatophilic virus which induces a series of immunologic reactions in the body. Because of disorder of immunologic regulative ability, endotoxemia and microcirculatory dysfunction, the liver cells are damaged liver function is impaired. Abnormal liver function can lead to regression of function of various systems of the body. The causes usually are:
(1) Hepatitis causes symptoms of gastrointestinal disturbance (such as anorexia, nausea, abdominal distention stomache ache, wetness-heat abdominal pain, gastro-intestinal hypersensitivity, constipation, diarrhea). It often affects the patient’s appetite and nutritional absorption. So, in chronic hepatitis, edema due to malnutrition is frequently encountered.
(2) Defect in protein synthesis (especially in albumin synthesis): Although the daily protein intake and absorption is normal, but if there is decreased synthetic ability of protein in the liver, the plasma albumin level would be low and also the plasma colloidal permeability is lowered so that mal-nutritional edema is likely to occur. (Lowering of plasma albumin is of diagnostic value, and 2.5% is considered as marginal level. In severe edema, the plasma albumin is usually below 2 g %).
(3) Hepatic coagulopathy: Liver participates with many coagulative functions of the body; besides vitamin K, it can also synthesize fibrinogen and thrombin. Decrease of hepatic function can affect the coagulation of blood and is likely to cause various kinds of acute or chronic bleeding. Clinically, the conditions often seen are subcutaneous ecchymosis (皮下瘀斑), hematochezia, epistaxis, hemorrhoidal bleeding, and, especially in female chronic hepatitis patients, irregular menstruation, menorrhagia, prolonged bleeding periods, dark color blood with numerous blood clots and repeated dysmenorrhea. During delivery, the bleeding is profuse and in operation or trauma, the blood loss is particularly excessive. Edema caused by repeated and prolonged chronic blood loss is a fact frequently encountered.
(4) Endocrine disorder: Liver is the target organ of many important hormones and is also the main site of hormone degradation, interchange, transformation, storage and excretion. Liver can synthesize sodium excretion factor, angiotensinogen (血管緊張素原) and erythropoietinogen (促紅細胞生成素原) and therefore it is also an endocrine organ. So, in hepatitis, hormonal disturbance is frequently induced, for example, hypothyroidism leads to myxedema (粘液水腫) and also, there may exist a rise of growth hormone and insulin. Pancreatic glucagonemia causes hepatogenic diabetes or hypoglycemia. At this time, the patient tends to be hungry easily and eat too much with the result of developing secondary obesity. Hyperestrogenemia and decrease of male hormone can be frequently seen in hepatic disease. A small number of male patients have breast development and feminine figure. If there is decrease of male sexual function in childhood, the patient tends to become fat and the external genital organ would also show significant underdevelopment.
(5) Abuse of hormones : The patient, because of long term extra-hepatic complications (such as asthma, german measles, eczema, osteal arthritic diseases like gout or erythematosus) used drugs like corticosteroids or sex hormones improperly (such as in treatment of infertility). In addition, before or after climacteric in male or female, it can also cause, in a short time, retention of water and sodium and subsequently induces edema, obesity and significant increase of body weight.
(6) Deficiency of B group vitamins: When there is dysfunction of liver, the patient’s thiamine acidifying ability decrease, the usage of vitamins B1 is interfered, the oxidative decarboxylation of pyruvic acid is impaired, so that the oxygenation process of glucose is affected. Further more, it affects the energy supply of nerve cells, leading to accumulation of pyruvic acid lactic acid in nerve tissues and subsequently, to multiple peripheral neuritis (多發性周圍神經炎) and wet beriberi (濕性腳氣) which produces edema.
In addition, some drugs may damage the liver and electrical therapy or chemotherapy may impair liver function and in such conditions, the patient’s edema may be aggravated. In clinical practice, it is often observed that long term administration of diuretics does not show marked effect in elimination of edema, but when TCM therapy is used, the edema regresses significantly or even completely disappears.
|
| Introduction of cases
Case 1 Run (code number 2027) female, age 32 years. First visit: December 1999. She complained of suffering from acute nephritis when she was 10 years old and it was finally cured. In the recent 5 years, she had edema which was more masked in the lower limbs. She received repeated TCM and WH treatment with no effectiveness. She had many times of physical examination and laboratory examination which ruled out cardiac and renal edema. Some physicians diagnosed it as endocrine disorder, but still the cause of edema was not clarified. At the onset of edema, she felt distensive pain in the lower limbs and afterwards, for a long period, she experienced tiredness, dreamfulness, poor sleeping, headache, abdominal distention, constipation and her body weight increased from 110 lbs to 130 lbs. She had irregular menstruation the amount of which was large with many blood clots and she occasionally had dysmenorrhea.
Physical examination: fissured tongue with red tip, medial furrow and white coating, face flushing, abdomen depressed without ascites, shrinkage of area of percussion dullness, liver lower margin 4.5 cm. above costal margin (3 finger breath above coastal margin), lower limbs with (+++) pitting edema more marked over dorsal surface of both feet, the latter showing extremely thin dorsal skin with transparency. (She brought her 1997 blood and urine examination reports, liver and spleen computer scan, chest and reprography x-ray film, but these did not reveal any abnormality ).
After taking 3 parcels of TCM drugs, shrinkage of liver dullness disappeared and through percussion the liver was actually enlarged to 1.5 cm with percussion tenderness. Another 4 parcels were taken and the liver was normal. She was treated afterwards by systemic TCM therapy and the edema gradually subsided, the clinical symptoms disappeared. She received TCM therapy for about 3 months and the edema of the lower limbs disappeared completely. Treatment was stopped after clinical cure and the patient was followed up.
|
| Case 2
Chan (code number 2832) female, age 67 years. Her first visit was on March 26, 2002 with the complaint of repeated abnormal sensation of lower limbs which included numbness, soreness, formication (蟻走感), burning heat sensation and paroxysmal pain of right gastronomies muscle. The latter condition caused persistent pain for two months with functional disability two years ago. Now the pain persisted for two more weeks and severe calf pain and fatigue attacked her for several days. Physical examination: haggard, puffy, flushing of face, tongue enlarged, lower limbs edema (+++), gastrocnemius muscle no significant tenderness, abdomen soft and distended, hepatomegaly of 1.5 cm.
After taking two parcels of TCM drugs, she had diarrhea, bowel movements 3 times in one hour amount large and stinking. When 3 parcels had been taken, edema of the lower limbs nearly disappeared and pitting edema was (+). The tongue was still enlarged but the liver was normal. Another week of TCM treatment gave her no pain in walking. In the course of treatment, she had occasional insomnia, fatigue, headache, acid regurgitation, stomache distention after meal and drawing pain of the diseased leg in walking. When going upstairs, pain was felt over the right gastroenemius muscle and in the third week of treatment, the right angle of lips showed vesicular eruptions. The symptoms disappeared when TCM treatment was going on. After 6 weeks of systemic TCM therapy, clinical cure was obtained and treatment was stopped for observation.
|
| Case 3
Yang (code number 2769) male, age 45 years. First visit: January, 2002. He complained of being a carrier of type B hepatitis virus for ten more years and he had a history of asthma in childhood. Twenty years ago, he had gastric hemorrhage and now he still felt upper abdominal distention and belching whether hungry or full. Gastroscopy revealed no abnormality. In recent years, he often experienced photophobia, dermal pruritus, fatigue, edema of lower limbs and early whiteness of hair which was dyed.
Physical examination: skin color dark, puffy, lips edematous with fissuring, After taking 3 parcels of TCM drugs, gastric discomfort was relieved; belching and flatulence stopped and the liver was normal. During the administration of TCM drugs, he experienced dryness of eyes, fatigue, sleepiness, dreamfulness, yellowish urine with foam, repeated belching, occasional diarrhea and pain of hypochondria (脅痛); edema of lower limbs disappeared. A total of 42 parcels of TCM drugs were taken, at the end of which clinical cure was attained. After that, he was followed up.
|
| Case 4
Lin (code number 2341) female, age 63 years. She first visited the clinic in January 2001 with the complaint of having fatigue, discomfort of heart, shortness of breath, itching of throat, coughing, shoulder and loin pain and insomnia for ten more years. Repeated drug treatment was not effective. She received hysterectomy (子宮切除) because of uterine myoma (宮肌瘤) ten more years ago.
Physical examination: puffy, skin palish yellow, tongue enlarged with medial fissure, tympanitic frog like abdomen, hepatomegaly of 1.5 cm, percussion tenderness over hepatic region, edema of lower extremities, pretibial pitting edema (+).
After taking 3 parcels of TCM drugs, the liver returned to normal. Her sleeping could last for five hours, but she still had mild vertigo and shortness of breath. One week later, the edema improved and fatigue disappeared. She had some itching of throat, occasional cough with abundant sputum and her sleeping was good. Mild vertigo occurred after waking up in the morning. She had bowel movement once in several days; the stools were hard. Blood pressure: 110/70 mmHg. The tongue was enlarged and liver normal. Edema of lower extremities disappeared. For the treatment of shoulder and loin pain caused by hepatic osteal malnutrition, she was given TCM therapy for nearly three months.
|
| By WONG Kwok Hung
Published on 20th June 2002 Translated by Professor Zheng in December 2004 |
Hepatogenic malnutrition and underdevelopment (One of the common symptoms of “deficiency of blood and weakness of qi”
| Chronic hepatitis can cause malnutrition and underdevelopment of the patient. In recent years, our clinic received many patients with abnormal margin of liver dullness, in which, those having marked “hepatogenic malnutrition and underdevelopment” numbered 136, occupying about 5% of the total 2862 cases. The proportion of females is larger (recent 3 years statistics the ratio of male to female is 7:22) in which the amount of patients under 18 years of age was 43, about 1/3 of the total “hepatogenic malnutrition and underdevelopment”. Those suffering from malnutrition and underdevelopment should be considered as cases infected during infancy or childhood. Therefore, attention should be drawn to prevention and treatment of pediatric liver disease. If TCM treatment is neglected before the adolescent period, the patient is likely to suffer “hepatogenic malnutrition and underdevelopment” throughout his life time.
Malnutrition is a syndrome caused by deficiency of various nutritional factors, and it displays differently in many kinds of disease. Thinness doses not absolutely indicate malnutrition, for example, simple hypoproteinemia, if severe, may give rise to edema, and in cases of endocrine disorder, contrarily, secondary obesity may occur. But malnutrition and underdevelopment would certainly lead to an under standard condition of “body height” and “body weight”. Therefore, a healthy figure does not actually relate to obesity, but concerns with the proportion of body weight to height, that is, the Body Mass Index. Body Mass Index, abbreviated as BMI, is the proportion of Body Weight (kg) to Body Height (M2), see Table 1 below: BMI = body weight (kg) / body height² ( m² )
|
|||||||||||||||||||||||||
Table 1: ideal range of BMI for teenages
|
|||||||||||||||||||||||||
Hepatitis in childhood Infection of “hepatophilic virus” during infancy and childhood is the chief cause of human malnutrition and underdevelopment. In daily life, the human body must absorb nutritious materials, such as, glucose, fat, protein, vitamins, inorganic salts and water for metabolic utilization, growth, development and activities of the body. Deficiency of the above nutrients may be caused by diseases, hypofunction of some organs leading to poor digestion and absorption, insufficiency and imbalance of nutritional factors or over utilization due to increased necessity of the body. Presently, due to the advance of knowledge about the pathogenic effects of “virus”, there are increasing evidences indicating that in many cases metabolic disorders, malnutrition and underdevelopment are caused by the infection of “hepatophilic virus”.
Liver is the axis of metabolism in the human body, its function is very complicated and certain functions of it, is closely related to the blood system, to glucose, protein, fat, water, electrolytes, vitamins and microelements. If the patient was infected by hepatophilic virus during infancy, the disease would affect the child’s nutritional absorption and cause anemia and endocrine disorder and interfere with his development. This forms “hepatogenic malnutrition and underdevelopment”. In the later growing years, the child would be weak and subjected to frequent attacks of diseases.
It is reported that in our country as well as in South-east Asia, the infection of type B and other hepatophilic viruses is very common, and the infection during infancy, childhood and early youth may persist for several or ten more years or even throughout life. Taking type B hepatitis as example, 70-90% of the patients would present prolonged positive reaction as “antigen carrier”, but have no clinical symptoms. Liver function tests demonstrate no abnormality but liver biopsy showed damage in 90% of cases. Although various types of hepatitis have different features in symptomatology, but hepatophililic virus infection invariably affects the child’s development and health. The child cannot help himself from being infected and some are infected even before delivery and the infection is destined to exist throughout his life. It is regretful that many parents and physicians do not pay much attention to pediatric virus hepatitis and often make misdiagnosis or miss the diagnosis in some way so that many children can not be diagnosed and treated in time.
Many chronic hepatitis patients were infected in the newborn or infantile period or during childhood, but their clinical symptoms unfortunately manifested late in the adult age and their diagnoses were suspected only at the discovery of abnormal liver function. With the pass of time, the majority of these patients developed chronic hepatitis, cirrhosis or carcinoma of liver. This reveals the fact that in recent years there is a tendency that victims of carcinoma of liver are becoming younger.
How to find out early that the child is suffering from hepatitis? This is what all parents wish to know. When there is chronic liver disease, the child has a lot of fire in the heart, liver and lung, and that heat in the large intestines is also abundant. If water in the kidney is consumed, the function of liver and kidney is affected. When hepatophilic virus entered the child’s body as pestilential evil, many clinical symptoms would be produced and it might lead to the formation of hepatogenic malnutrition and underdevelopment.
The TCM viewpoint is that kidney stores essence of life, regulates growth, development and fertilization. The vital essence and energy is a basic material of the human body and is also a fundamental substance responsible for growth, development and many activities of the body. The vital essence and energy stored in the kidney includes “the congenital essence of life” and “the acquired essence of life”. The former occurs with the beginning of life and the latter comes from ingestion of food which is transferred into water and nutritional elements by spleen and stomache. It intermixes with the genuine energy produced by the physiologic activities of zang and fu organs, and through metabolic regulation and balance, the remaining parts are stored in the kidney. So, the vital essence and energy in the kidney is the basis of life activities and the physiologic effect of kidney vital essence and energy can include kidney yin (nourish and lubricate various tissues and organs of the body) and kidney yang (activate and warm various tissues and organs of the body). The two of them rely on, restrict and take advantage of each other. At the same time, they maintain relative balance of yinand yang of various zang and fu organs. Therefore, it is said, in TCM, that kidney dominates bone and generates bone marrow. In fact, the vital essence and energy within the kidney is an important component in promotion of developmental function of the body. But, in liver disease, the dysfunction or failure of liver and kidney, provides opportunity for the evil (or virus) to damage the regular metabolic procedures. As the TCM principle denotes, the development of bone depends on the fullness of bone marrow together with the nourishment provided by it. When the virus evil invades and causes functional deficiency of liver and kidney, general metabolic disorder is produced, and if the condition is not treated in time, it will become serious and invariably lead to malnutrition and underdevelopment.
It is commonly known that chronic virus hepatitis is a generalized disease and individuals of unlike constitution, in different periods of life, may present symptoms of different systems. In pediatric virus hepatitis, the hepatitis virus might have attacked the body early during infancy or childhood and directly or indirectly affected all the organs of the body. Immune compounds (antigen-antibody compounds) may form and deposit on the lymph nodes, spleen, vascular endothelium, renal glomerular basal membrane, sensorial membrane and vascular networks, and produce inflammatory and degenerative changes, and in clinical practice, two kinds of hepatitis can be seen, the “chronic persisting hepatitis” and “chronic active hepatitis”. The former is due to decrease of the child’s immune ability so that the hepatitis virus can not be eliminated causing the disease persisting and hard to be cured; the latter is formed because of defect of immunologic function and deficiency of antibodies, so that the virus can not be entirely eliminated and its replication is not inhibited. There are still some liver cells continuously destroyed under the action of hypersensitive lymphocytes and subsequently the disease runs a prolonged uncured course, leading to damage of many systems in the body and presentation of different clinical symptoms.
Besides chronic hepatitis, patients suffering from acute nonicteric hepatitis, subclinically infected individuals or patients with concealed infections may present mild, insignificant or no symptoms. If we can diagnose the child suffering from virus hepatitis in time, he will be treated in time. The former standard of diagnosing chronic hepatitis (such as the existence of antigen, antibodies and liver function abnormality by blood examination, positive result by ultrasound or computer screening) is extremely inadequate and it will certainly produce large amounts of misdiagnoses and missed diagnoses. The physician can diagnose and treat the disease in time if he is familiar with the TCM classification and symptoms of chronic hepatitis and the finding of abnormal margin of hepatic dullness. In the 2855 cases of abnormal margin of hepatic dullness recorded in our clinic during these years, there were only 895 cases confirmed according to the diagnostic criteria of hepatitis, occupying 31.3%. The remaining 2000 cases (about 70% of the patients) had only chronic hepatitis clinical symptoms and abnormal margin of hepatic dullness. If they were given effective systemic TCM treatment, clinical cure should be the expected result.
|
|||||||||||||||||||||||||
|
Symptoms of hepatogenic malnutrition and underdevelopment
The most common symptoms in children with chronic hepatitis are thinness, dullness, fatigue, polish yellow or polish white of skin, pale mucous membrane of eyelids, lips and tongue, dryness of skin, hyperkeratosis, scaly desquamation and fissure formation. The patient is susceptible to eczema, varicella and sweat stains. Because of the decrease of immunologic ability, the patient is also extremely susceptible to infection. Some pediatric patients tend to develop abnormal psychotic behavior such as anxiety, insomnia or reticence, indifference to the surroundings, retardation of memory and childish actions. Manifestations of malnutrition in children include soft and distended abdomen, shallow and flat umbilicus (or even protruding), scarce subcutaneous fat, skin easily picked up by fingers, If hypoalbuminemia is marked, one may find edema of the ankles and finger marks over the pretibial region (pitting after finger pressure).
Being parents, they must recognize and take preventive measures against hepatophilic virus infection during their child’s infancy and must give thorough treatment to liver disease, if present; this is the only way to ensure the child’s health. This is also a basic method of improving the body constitution of the population in our country. Once the development of hepatogenic malnutritition and underdevelopment has taken place, the patient’s health may be affected for a life time.
|
|||||||||||||||||||||||||
| Case 1
Yang (code number 0453), male, age 4 years. He was born on 6th November 1997 and first visited our clinic on 14th September 1998. His father had chronic hepatitis. The child’s complaint was substituted by his mother who said that her son often had pruritus and dryness of the skin, nocturnal crying and had a hepatomegaly of 1.5 cm. Because at that time the child’s age did not exceed one year, she did not dare to give him TCM drugs. His return visit was on 30th August 1999. His mother said that he still had skin eruptions and repeated erythema, edema and pruritus of the skin which also showed fissures and exudative ulcerations. He had bowel movements ever two to three days; the stools hard and bleeding occurred after defecation. The child was dysphonic and had feeling of tiredness. Physical examination: pallor of face, malnourished and underdeveloped, weight 22 lbs, skin dry with desquamation and infantile eczema, liver still enlarged to 1.5 cm. Diagnosis: hepatomegaly for investigation, hepatic malnutrition and underdevelopment, rectal varicosities, anal fissure complicated with hemorrhage, virus gastrointestinal disease, xerosis cutis syndrome, eczema, rubella.
After taking 7 parcels of TCM drugs, the liver returned to normal, hematochezia stopped, but there was still constipation and fatigue. The xerodermatic lesions improved. TCM drugs were continued for 4 weeks at the end of which clinical cure was attained and medication was stopped for observation.
|
|||||||||||||||||||||||||
| Case 2.
Wang (code number 2289) female, age 41 years. Her first visit was in December 2000 and she complained of being a carrier of type B hepatitis virus for 10 years and had repeated exopathic coughing, nasal obstruction, copious expectoration, epistaxis and fatigue. There were facial pigmented patches since ten more years of age. In the recent three months, cough was more conspicuous; she often felt pain in the chest, low grade fever, headache, bowel movements 1-3 times daily, often associated with bleeding.
Physical examination: thin, malnourished and underdeveloped, thirsty, weight 40 kg, height 1.54 m, BMI 16.8, telangiectasis over medial side of both popliteal fossa, marked hypochondriac anomaly, percussion tenderness over hepatic region, hepatomegaly of 4.5 cm.
After taking 3 parcels of TCM drugs, the liver was normal and she slept well and had no headache. She still felt thirsty, the nasal discharge was yellowish and viscous; there was nasal obstruction, occasional coughing, fatigue, sleepiness and bowel movements twice a day with tenesmus. The pulse was 108/min. After another 4 parcels of TCM drugs, the common cold alleviated and coughing stopped. There was some chest pain and examination revealed localized tenderness over the sternocostal joint. She persisted in taking TCM drugs and during the course of treatment, cough, itching of throat, abundance of sputum, fatigue and tenesmus all gradually disappeared. A total of 42 parcels of TCM drugs were taken. Clinical cure was achieved and therapy was stopped.
|
|||||||||||||||||||||||||
| Case 3
Lin (code number 2031), female, age 18 years. Her first visit was on 1st January 2000 with the chief complaint of having a history of repeated gastritis and enteritis associated with repeated nausea, vomiting and loss of appetite. She now became thin and suffered frequently from cough, with large amount of sputum, headache, chest pain, liver pain and generalized pain of the bones. She had occasionally cold and fever and nocturnal perspiration. She was diagnosed as pulmonary tuberculosis and treated by western medicine. But during the anti-tuberculosis treatment, blood examination revealed a high ferment, so that, for two times, the therapy was stopped. Now she asked for TCM to treat her liver illness.
Physical examination: lean, body weight 40 kg, height 1.52m., BMI 17.3, skin color polish, anemic looking, female secondary sexual characteristics under-developed, tongue reddish, coating thin and yellow, pulse 104/ min, abdomen navicular, percussion tenderness over hepatic region, hepatomegaly of 3 cm. After taking TCM drugs, she experienced abdominal pain, diarrhea and flatulence, burning pain of anus, abundance of sputum and coughing. The liver returned to normal after taking 3 parcels of TCM drugs, and the pulse was 112/min. She totally took 14 parcels of TCM drugs and then stopped the therapy for 11 days. She visited again because of asthma and cough, abundant sputum, abdominal distention nocturnal perspiration. Physical examination revealed an enlarged liver of 1.5 cm which formed the first relapse. Six parcels of TCM drugs were required to bring the liver to normal. During the course of systemic TCM treatment, the symptoms disappeared gradually. The course of treatment was 6 week; clinical cure was achieved and the patient was followed up.
|
|||||||||||||||||||||||||
| Case 4
Chan (code number 2038), female, age 17 years. His first was on 10th January 2000. She complained of repeated wetness-heat abdominal pain since childhood and also constipation, bowel movements every three or four days with hard stools. She had to defecate right after meal, and frequently suffered from wetness-heat, abdominal pain and tenesmus. Her menstruation had a lag of about 10 days every time, the amount not large and the color bright red; pain was present. For a long time, she had acne over the face, being more marked in the period before and after menstruation.
Physical examination: limbs long, thin, poorly nourished and developed, skin dry, numerous sweat stains, hairy lower limbs, toque reddish, prominent taste buds, toque enlarged with teeth prints, thick yellowish coating, finger nails pale, secondary sexual characteristics underdeveloped, hypochondriac anomaly, hepatomegaly of 1.5 cm, percussion tenderness over hepatic region, body weight 43 kg, height 1.64 cm, BMI 15.98.
After taking 4 parcels of TCM drugs, the liver returned to normal. She took totally 3 weeks of TCM drugs and stopped the medication by herself, although the course of systemic treatment was not ended. She returned to the clinic two months later complaining of sorethroat, coughing for several days with chest pain and constipation.
Physical examination revealed hepatomegaly of 1.5 cm. which was the first relapse. She was given 3 parcels of TCM drugs, after which the margin of hepatic dullness became normal. She had again systemic TCM treatment for 6 weeks and it resulted in clinical cure. She was followed up and was advised to take hormone replacement therapy which gave her prominent changes of secondary sexual characteristics and improvement of nutrition and development.
|
|||||||||||||||||||||||||
| Case 5
Zhang (code number 2152), female, age 33 years. First visit: June 2000. She was thin since childhood and ate little, body weight being 35 kg, height 1.5 cm and BMI 15.5. She suffered from neurosis, anorexia and failed to increase body weight in spite of receiving information from a nutritionist. For a long time, her appetite was poor and she often had tiredness and insomnia and because of the latter, she was given hypnotics and anti-allergic agents. She was susceptible to headache and sorethroat. In recent years, she often had belching, distensive pain of abdomen, diarrhea and stomache ache which aggravated half a year ago and required gastroscopy but the result revealed no abnormality. She had irregular menstruation (once in about 30-40 days), lasting for 6-10 days with clots and dysmenorrheal which required calling for emergency once. Physical examination : polish yellow color of face, wan and sallow looking, anemic and lean, underdeveloped, tongue enlarged with marginal teeth prints, mild percussion tenderness over hepatic region, hepatomegaly of 4.5 cm, mild edema of lower extremities, prominent veins and mild venous varicosities of lower limbs. The diagnosis was chronic hepatophilic virus disease, hepatomegaly for investigation, hepatic malnutrition and underdevelopment, hepatic anemia, anorexia, hypotension, hepatic neurosis, sexual hormone disorder, hypertension of inferior vena cava, venous varicosity, hepatogenic peptic ulcer, virus gastrointestinal disease, menstrual disorder, dysmenorrheal, hepatic edema, hepatophilic upper respiratory tract infection.
After taking two parcels of TCM drugs, bowel movements were smooth but the amount of stools was small. Her appetite improved, and sleeping was good but could be easily awaked. Her hepatomegaly shrank to 1.5 cm; the blood pressure 82/50 mmHg; lower extremities edema (+). After another 3 parcels, the liver was normal. The menses appeared two weeks after the medication and the amount had a decrease of one third. On the fourth day of menstrual flow, the amount reduced (in former months, it needed 6-7 days); there were no clots but dysmenorrheal still existed which required analgesics for 5 times in the first two days. Clinical cure was obtained after taking 48 parcels of TCM drugs.
|
|||||||||||||||||||||||||
| General knowledge about liver disease
Symptoms induced by metabolic disorder commonly seen in liver disease
When infection of hepatophilic virus has led to parenchymatous hepatic changes, various metabolic disorders may be evoked; the following are the ones usually encountered.
Children with chronic hepatophilic virus disease are usually infected through the mother-child pathway or by close contact, therefore infantile hepatitis causes malnutrition and the development of some children may be affected. The hepatic metabolic function of children is weaker than adults, its protein synthetic function is lower and when the liver is injured, there is synthetic insufficiency of albumin, fibrinogen and coagulative factors. Therefore, children with chronic hepatitis often have hypoalbuminemia, disturbance of calcium absorption and bleeding tendency. In there is decrease of growth hormone in the blood due to endocrine disorder, the diseased child would have calcium deficiency and form bone malnutrition. The cause lies on the fact that chronic liver disease induces nausea, vomiting, poor appetite and gastrointestinal disturbance, affecting absorption of various nutrients. Inflammation can also cause decrease number of hepatic cells and lowering of hepatic function, inadequate food intake and decrease of synthetic ability. All these can easily lead to hypo-albuminemia and production of nutritional disturbance and subsequently to malnutrition and underdevelopment.
Clinically, the pediatric patient’s abdominal wall is soft and distended, and it shows prominent venous collateral circulation and telangiectasis. The patient’s liver is usually enlarged; right hypochondriac pain can be shown in larger children and during examination hepatic percussion tenderness can be detected. The child may have bleeding tendency and present repeated epitasis, hematochezia, bleeding of the gums and history of spontaneous or postcontusion ecchymosis.
At present, it can often be found clinically that if one was attacked by hepatitis during infantile and childhood, he may show by examination, during the school age, young or middle adult age, asymmetry of the hypochondria, the left hypochondria slightly depressed or protruding like an angle, the right hypochoridrium full, extending outwards or even bulging.
In medical practice, there is a formula for calculation of a child’s body weight to know whether it is up to standard or not; it under standard, it means the body weight is insufficient. This formula is: Age in year x 2 + 7 = body weight of child in kg.
It is a series of bone pathologic changes induced by metabolic disturbances of calcium, phosphorus of Vitamin D in liver disease, including chiefly diseases like osteoporosis, rickets and osteomalacia. A small number of cases may develop into “hepatic dwarfism”. The diseased child’s face is lack of luster; he is smaller than general, lean, growing much more slowly and the inadequate calcification of bones leads to rickets. In severe cases, there are costal moniliformis, chicken breast; anomaly of spinal column, chest and feet. This is due to endocrine disorder in chronic hepatitis which causes lowering of the level of growth hormone and also calcium deficiency; this subsequently results in osteal malnutrition. When anomaly has taken place, the result of operative correction is usually not ideal. If the patients’ chronic hepatitis can not be treated thoroughly with systemic TCM method and not cured clinically, operative treatment can only be “a measure for the superficial and not for the fundamental”.
Hepatogenic hypoglycemia often aggravates progressively in its degree of severity and frequency of attack. It tends to attack before breakfast, the meal time is then delayed and fasting may be induced. Its manifestations include getting hungry easily, palpitation, perspiration, tremor of hands, pallor of face and anxiety. The more serious cases may have dizziness, headache, blurring of vision, slowness of response or even hypoglycemic encephalopathy such as psychosis.
In liver disease, metabolic disturbance of potassium presents as hypokalemia, which is caused by inadequate absorption, vomiting or diarrhea. Clinically, these are myasthenia oliguria, anuria, bitter taste, loss of appetite, distention of abdomen, hypotension and, in severe cases, restlessness, emotional instability and sleepiness.
The clinical symptoms of this entity include haggard looking, weakness, indifference, loss of appetite, thirst, anxiety, dizziness, distensive feeling of head, headache, anorexia, nausea, vomiting, paleness and coldness of limbs. In severe cases, these are painful spasm of muscles, blurring of vision, hypotension and postural collapse.
An early symptom of pediatric diabetes is infantile nocturia which is acute in onset and once discovered it is usually quite serious. It is often associated with thinness, polydipsia, polyuria, polyphagia, hunger, fatigue and unlively behavior. The patient is susceptible to infections. If the disease is prolonged, the child may present xeroderma, scaly desquamation, pruritus or hairiness.
|
|||||||||||||||||||||||||
|
Soup recommendation
“Large snail meat and pork calf yin nourishing soup”
TCM theory acknowledges that food and medicine are of the same origin. In addition to systemic TCM therapy, during the course of treatment or after clinical, hepatophilic virus disease patients are advised to take the “nourish yin and supplement kidney” soup from time to time. It renders the kidney to hold plenty of water so as to suppress the initiation of heart fire, liver fire and lung fire. The body constitution of the hepatophilic virus disease patient belongs to the category that is deficient but not suitable to be supplemented; therefore, the soups with dryness heat or with coldness character should not be taken,
[Materials] One large snail or frozen snail head half lb, pork calf 500g, Poria, Semen Eurgales, Rhizoma Dioscoreae, Peeled white Semen Nelumbinis in small amounts, mushroom, 6-8 pieces, one piece of raw ginger, a bit of table salt.
[Method] 1. Large piece of pork calf placed in boiling water for a very short time. 2. One piece of fresh snail, remove, the shell and viscera together with the dirty attacked parts. Clean with water. If the snail is refrigerated defrost and clean it. Remove water for preparation. 3. Put all materials in cooler, add adequate amount of boiled water, increase intensity of fire to boiling degree, then use moderate or small fire to maintain boiling 2-3 hours, add some table salt for flavoring.
[Effect]
|
|||||||||||||||||||||||||
| By WONG Kwok Hung
Published on 30th May 2002 Translated by Professor Zheng in November 2004 |
|||||||||||||||||||||||||
Hepatogenic Anemia One of the common symptoms of “Deficiency of blood and weakness of qi”
|
Chronic hepatophilic virus disease inevitably gives rise to “deficiency of blood and weakness of qi“because liver is the axis of metabolism in the human body and also is an organ indispensable to the maintenance of life. Liver function is very complicated, and certain functions are closely related to the blood system. So, in liver disease, there are often hematological changes which may be simple abnormality of blood cells or mild coagulopathies (but in serious liver diseases, severe coagulopathies are quite common and they are often the main causes of death in patients with hepatic disease). In addition, there may be decrease of all blood cells or generalized hemorrhages in the whole body, or even failure of the entire bone marrow such as in fulminant hepatic failure and the patient’s death can be caused by the complication of disseminated intravascular coagulation. “Hepatogenic anemia” is very common, and it is reported in the literature that anemia, in liver diseases of various causes, reaches 77.3%. Although hepatogenic anemia occurs commonly, but often times, it remains unnoticed due to the undefined diagnosis of hepatitis or concealed under the cover of symptoms of liver disease. Up to the present, not few physicians still consider “hepatogenic anemia” as anemia of unknown etiology and the result is probably long term misdiagnosis. In fact, the principle of treating hepatogenic anemia is treatment of liver disease in the first step and increase of nutrition to improve liver function and subsequently the blood disease may also improve. If chronic liver disease is not detected and confirmed early and not treated in time with systemic TCM therapy to achieve clinical cure, the course of disease would continue, the functions of internal organs are continuously impaired and the extra-hepatic complications such as anemia would increase day by day, and recovery is more difficult. We have received 2787 chronic hepatophilic virus disease patients; in this group there were 457 patients (16.4%) who presented symptoms and signs of hepatic anemia. In these patients, male were 997, in which only 46 patients had hepatic anemia, being 4.61%, which in 1790 female patients, anemia occurred in 411 patients, reaching 22.96%. Etiology and pathoginesis of hepatogenic anemiaFrom the TCM point of view, virus, the pestilential evil, on entering the human body, can hide itself as in “evil” in the blood and attack the internal organs – five zang-organs and six fu-organs. The “evil” not only hurts the body energy and resistance, but also disturbs the qi and blood. If here is dysfunction of the zang and fu organs, the blood would inevitably flow in the adverse direction and leave the body and the body would become more susceptible to deficiency and to damage of qi and blood. If treatment is not proper or if there are depression of qi, menorrhagia, mental consumption, fatigue of heart and kidney, large amount of blood loss and little blood regeneration, the pathological conditions of deficiency of both qi and blood would gradually occur. With the advance of science, the knowledge about hepatophilic virus disease has been much increased and it is known that the etiologic factors of hepatogenic anemia may act singly or in a complex manner, such as:
1. Malnutrition and decrease of storage of hepatic hemopoictic factors:Loss of appetite and decrease of absorption in the intestinal tract in chronic hepatitis patients can directly cause protein metabolic disorder and hypoproteinemia, affecting not only the synthesis of plasma albumin by hepatic cells, but also the production of hemopoietic factors like folic acid, leading to deficiency of iron and finally to the formation of anemia. The liver stores vitamin B12, folic acid and iron, so liver disease would definitely lead to decrease storage of these hemopoietic factors and subsequently to anemia. Alcohol can directly interrupt the absorption, metabolism, hepato-intestinal circulation and usage of folic acid; therefore, liver disease patients must stop drinking.
2. Chronic blood loss:Liver disease may be associated with clotting defect and therefore it provides a high risk to hemorrhage. According to statistics, 85% of liver diseases have at least one item of coagulation abnormality and 15% present a bleeding tendency. Therefore, hypodermic purpura, epistaxis, hemoptysis, menorrhagia, gastrointestinal bleeding, rupture of hemorrhoid and esophageal veins, parturient and postpartum periods may all cause hemorrhagic anemia.
3. Hemalysis:In liver disease, the life time of the patient’s red blood cells is shortened; this indicates hepatic anemia is related to hemolysis. It is commonly considered that in liver disease, the increase of cholesterol and phospholipids deposits on the cell membrane of red blood cells and the decrease of GSH inside red blood cells are related to splenic hyperfunction.
4. Increase of plasma volume:In liver disease, there is significant increase of plasma volume due to hepatic edema and cirrhotic ascites and it subsequently induces dilution of the blood.
5. Decrease of hemopoietic function of bone marrow:Hepatic dysfunction causes decreased production of prodromal substances of red blood cell genesis and therefore affects bone marrow hemopoiesis. (Alcohol can also directly inhibit bone marrow red cell generation, so liver disease patients must stop drinking).
Symptoms of hepatogenic anemia
Due to the complicated clinical symptoms of liver disease, the symptoms and signs of hepatogenic anemia often belong to different forms TCM classification. For example, anemia may be caused by chronic hepatitis, and although chronic hepatitis may not be confirmed by blood examination, ultra-sound or computer screening, it is still possible to discover signs such as abnormal margin of hepatic dullness during physical examination. The causes of anemia from liver diseases are many, and through statistical data, one can also find that hepatogenic anemia often includes various clinical kinds of anemia, such as, megaloblastic anemia, occupying 32.6% (mainly folic acid deficiency), normoblastic anemia 30.3% (mainly due to hemolysis), microcytic hypochromic anemia, 14.4% (mainly due to iron deficiency) and aplastic anemia, 0.06%. In hepatic anemia, there are also some manifestations commonly seen in anemia, such as vertigo, dizziness, palpitation, insomnia, dreaminess, sleepiness, fatigue, coldness of limbs, sluggishness in speaking, pallor of face and headache due to deficiency of blood. If there is prolonged deficiency of yang, entrapment of wetness and hepatic edema, secondary obesity may occur. Introduction of cases
Case 1. Zheng (code no. 2126) female, age 44 years. First visit: May, 2000. Her chief complaint was that she was a carrier of type B hepatitis virus for 10 years. She was puffy since childhood and often experienced fatigue, nasal hypersensitivity and shortness of breath. The menstruation was irregular with occasional dysmenorrhea and the blood amount was extremely large, the bleeding rapidity may cause a menstrual pod soaked up thoroughly in 1-2 hours. Because of this, she dared not move much during menstruation to avoid excessive bleeding. In the postmenstrual period, she often had repeated headache and common cold. During the visit, she was having sorethroat and hoarseness of voice for a week, associated with cough and viscous sputum. Her figure belongs to the obese type, weighing 140 lbs, height 5 feet 2 inches. Her tongue was enlarged with teeth prints, lower extremities pitting edema (+), percussion tenderness over hepatic region, hepatomegaly of 3 cm. The diagnosis was active chronic hepatitis, liver stagnation and lung dryness, with TCM classifications of deficiency of blood and weakness of qi, blockage of channels and stasis of blood, hepatic edema, secondary obesity. After taking 3 parcels of TCM drugs, the liver was normal. Hoarseness and coughing improved, there was no sputum, but the passing out of flatus was frequent. The tongue was still dry with red margin and thin coating; edema of lower limbs disappeared. She took another 4 parcels and the sorethroat and coughing disappeared. There was mild diarrhea; the stools were loose and copious. After one week of TCM medication, the menses appeared and its amount significantly decreased, but the color was bright with little clot and no dysmenorrhea. The liver was still normal and the lower extremities showed mild edema. During the course of TCM therapy, there was occasional sneezing and nasal discharge. Abdominal pain before defecation was still present; and bowl movements appeared every other day. The tongue was still enlarged and edema over the lower limbs was (+). Systemic TCM therapy lasted for 4 weeks and the patient did not feel any discomfort. Edema of the lower extremities was minimal. Clinical cure was attained and TCM therapy was stopped for observation. Menstruation reappeared after stoppage of treatment and its color was brownish red, the amount of blood decreased markedly. It lasted for 3 days without dysmenorrhea and blood clots. |
| Case 2
Yi (code no. 472) male, age 43 years. First visit: October 1996. He complained of suffering from acute type A hepatitis 20 years ago and was treated in hospital. He had a history of stomache illness since childhood and was once hospitalized because of bleeding and received blood transfusion. In the recent 2 years, he often had palpitation, vertigo, tremor, feeling of weakness and insomnia. He was diagnosed as anemia and neurosis. Physical examination revealed anomaly of hypochondria, percussion tenderness of hepatic region and hepatomegaly of 3 cm. His lower extremities showed (+) pitting edema. He was treated with systemic TCM, resulting in disappearance of symptoms and clinical cure. He was reexamined in September 1997 and his liver was normal and he did not feel any discomfort.
|
| Case 3
Lee (code no. 061) female, age 26 years. First visit: July 1998. She had a history of Mediterranean anemia, and urinary system infection. She often had vertigo, abdominal distention and diarrhea. Her menstruation was regular, the color bright red, large in amount with many blood clots. Physical examination: color of face palish fellow, anemic, thin, wan and sallow looking, tongue enlarged and pale with marginal teeth prints, abdomen soft and distended, protuberance of right hypochondrium and depression of left hypchondrium, hepatomegaly of 3 cm, mild edema of lower extremities. She was diagnosed as hepatomegaly for investigation, hepatopathic upper respiratory tract infection, hepatogenic peptic ulcer, virus gastrointestinal disease, hepatogenic anemia, menstrual disorder, urinary system infection.
After taking 6 parcels of TCM drugs, the liver returned to normal and symptoms also disappeared. During the course of systemic treatment, the liver was enlarged to 1.5 cm in the postmenstrual period in August and it became normal after taking another 3 parcels of TCM drugs. When the systemic treatment ended, clinical cure was attained and the patient was followed up.
Four months later, she was hospitalized for 5 days because of fever and urinary system infection. She received oral cephalosporin and anti-inflammatory drug injections. Physical examination after discharge from hospital revealed hepatomegaly of 4.5 cm, which was the first relapse of liver enlargement. Three parcels of TCM drugs brought the liver to normal. Systemic TCM therapy was given and clinical cure was attained afterwards.
Thereafter, the patient received persistently TCM therapy before each menstrual period and was followed up uninterruptedly. Anemia was corrected and she felt no discomfort. During the four years of observation, hepatomegaly relapsed for 6 times (once after taking durian and shousi, once after uncooked lobster, once after traveling to Korea for 5 days, the remaining two times cause not clear), but all were cured by systemic TCM therapy.
|
| Case 4
Chan (code no.527) female, age 18 years. Her first visit was in June 1994.
She complained chiefly of marked thinness recently, the body weight dropping from 96 lbs to 89 lbs within several months and also insomnia and yellowish urine for half a year. In the recent 10 days, she had repeated vaginal and the menstrual blood was red or brownish and large in amount. She also experienced vertigo, nausea, perspiration, palpitation and a pulse rate of 100/min. Physical examination: thin and anemic, pale color of face, tired looking, hepatomegaly of 4.5 cm with percussion tenderness. After taking 6 parcels of TCM drugs, the menstrual blood amount decreased and color became red. The liver shrank to the costal margin. Another 3 parcels of TCM drugs brought the liver to normal. Her menstruation was normal; her sleeping and mental condition was good.
After 9 parcels of TCM drugs, her menses appeared but the liver was enlarged to 3 cm and another 3 parcels of TCM drugs brought it to normal. Her menses lasted for 6 days and TCM drugs were taken every month before and after menstruation since the termination of the TCM therapeutic course. Thereafter, the menses were regular and no hepatomegaly or clinical discomfort occurred during menstruation. Her last return visit was on 12 June 1996, at which time them was no hepatomegaly, her anemic condition improved and the menstruation was normal.
|
| Case 5
The Leung sisters.
Their body build were of the weak type; they were examined and suspected to have Mediterranean anemia and treated with WM drugs. Their mother had a history of positive type B hepatitis antibodies by blood examination, Leung (code no: 545) female, age 25 years. Her first visit was in June 1996 with the complaint of getting tired easily, especially during the menstrual period. She experienced headache post-menstrually. Physical examination: marked anemic appearance, polish color of mucous membrane of lips, tongue and eyelids, blood pressure 90/50 mmHg, abdomen soft, hepatomegaly of 3 cm. After taking 6 parcels of TCM drugs, the liver shrank to the costal margin and after another 3 parcel, the liver was normal. Sometime TCM therapy lasted for 6 weeks and medication was stopped when clinical cure was attained. A return visit was made 8 months after cessation of medication and it was found that the anemia was corrected significantly. No clinical symptoms appeared and liver was normal.
Physical examination revealed a marked anemic figure; the mucous membrane of eyelids, lips and tongue pale like paper, the tongue enlarged with teeth prints, the lower extremities slowing (+) pitting edema. After taking 9 parcels of TCM drugs, she could sleep but wakeful and her liver became normal. The visit happened to be the 2nd day of menstruation, the color was bright red, the clots were few and no pain was present. TCM treatment continued for three months; during this period, there was occasional vertigo, repeated ulceration of the mouth and pharynx. The stools were of the wetness-heat character. In each premenstrual period, she felt distention of the breasts, but no dysmenorrhea. The menstrual blood was bright red, the amount less and without clots. At the stoppage of medication, she was well, her sleeping was good, her appetite was normal and her anemia had been corrected significantly. Her lips were red and she felt no discomfort. In the following months, she received TCM therapy during thee premenstrual days and she felt no discomfort, the liver was also normal,
Six months later, she made a return visit because of exapathy for 3 days. She was afraid of relapse of the liver disease. Physical examination revealed a hepatomegaly of 1.5 cm. She was treated by systemic TCM therapy which was stopped at the attainment of clinical cure.
|
| General knowledge about liver disease
Hepatitis aplastic syndrome
A small number of hepatitis cases (especially acute icterohepatitis) may develop aplastic anemia, also called “hepatitis aplastic syndrome”, during the course of the disease or in the period of convalescence. The incidence is higher in pubescent and young people. And about 90% occur in the year following onset of the disease. According to statistics, hepatitis aplastic syndrome occupies 1.07% – 5.8% of aplastic anemia and those complicated by aplastic anemia account for 0.34% – 0.4% hepatitis cases. There are about 0.06% – 0.07% of children with hepatitis complicated by aplastic anemia.
The aplastic anemia cases following hepatitis are usually severe ones, and their conditions may aggravate rapidly. Their clinical manifestations include the three major categories: anemia, bleeding and infection, and the main causes of death are intra-cranial hemorrhage and septicemia.
To avoid hepatitis aplastic anemia, when hepatitis is confirmed, it is necessary to administer at once systemic TCM therapy to achieve clinical cure. This can prevent direct injury to the hemopoietic stem cells by hepatitis virus, inhibition of hemopoieses by immunologic reactions and decrease of hepatic detoxification function.
|
| By WONG Kwok Hung
Published on 25th April 2002 Translated by Professor Zheng in October 2004 |
TCM Treatment on Erythematous Lupus
Erythematous lupus is not unusual and is often found among women. Traditionally, people believed that there is no way to cure cazenaves lupus and it would easily cause disturbance of the functioning of the liver and kidney system and would eventually lead to death. People who were diagnosed as having cazenaves lupus are therefore very worried and seemed like having been sentenced to death.
In traditional Chinese medical science, it is believed that “red butterfly sore” (namely cazenaves lupus in western medical science) is caused mainly by the deficiency of the inborn congenital energy and the impairment of the liver and kidney. It is because the liver is responsible for the storage of blood while the kidney is responsible for the storage of the vital energy (“qi”). When both the vital energy and blood are insufficient in supply, it would easily cause the hyperactivity of fire in the body due to the deficiency of yin and the up-float of yang. In addition, because of incompact muscular striae, pathogenic factors would attack the body through our skin. Once the heat evil entered the interior, our venation would be blocked and cause damages to viscera interiorly and forms external blockages in the skin. This article focused on the treatment of cazenaves lupus using traditional Chinese medicine and that such treatment should start with the liver organ.
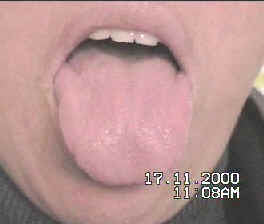
<Figure 1 and 2 are the comparisons about skin erythema, tongue and lip-mucosa pathological changes before and after treatment of Case 2>
Acute symptoms
In fact, erythema-like skin injury is usually the clinical symptoms of lupous hepatitis. Lupous hepatitis is one type of chronic active hepatitis. It is probably related to the body immunity system and it would usually occur in young female. During the acute period, the common symptoms are icterus, fever, inflammation of the liver and spleen, skin rash, spider angioma, arthritis and ascites. In some cases, it may be supervened with nephritis, colitis, myocarditis and stomatitis. Blood tests may find lupus cells in some patients and that their liver function test usually shows liver function disturbance, for example, serum gammaglobulin, glutamic-pyruvic aminotransferase (GPT), alkaline phosphatase (AKP) and bilirubin increases apparently.
Chronic symptoms
Besides the acute symptoms, patients with chronically hepatitis usually show symptoms like listlessness, fullness of the abdomen, diarrhea, skin pruritus, skin rash (mainly erythema), dysmenorrhea, menses disturbance, amenorrhea. Sometimes symptoms like hyper-adrenocorticism may appear, such as physical sign of obstinate acne, purple striae, hepatic edema, secondary obesity and moon-face. It is also easily supervened with immunity diseases of other systems (such as ulcerative colitis, polyarthritis, glomerulonephritis, and so on). In fact, these symptoms are often found in the clinical manifestation of different types of viral hepatitis.
The following cases are patients having negative result in testing hepatitis virus. However, it cannot exclude the possibility of virus infection even if it showed a negative result. As we applied a systematic traditional Chinese medicine treatment in terms of viral hepatitis, the result is always quite effective. Patients who are diagnosed as cazenaves lupus should have the possible attitude that by using a systematic traditional Chinese medical treatment, it can be clinically cured. The following two cases are related to cazenaves lupus.
<Figure 3 and 4 below are the comparisons about the pathological changes of the tongue before and after treatment of Case 2.>
| Case 1
Zhao X (computer number 2123), female, 51 years old. First visit was made in April 2000. Her chief complaints were: She suffered ailment from childhood, born two boys and one girl, got induced abortion twice and natural abortion four times. She has had amenorrhea since last year, often in perturbation. She had her menstruation once this year soon after taking traditional Chinese medicine. She got chest pain, short breath, and “foreign body sensation in throat” five years ago and had undergone physical examination. Lupus erythematosus cells were found in blood test and computer scanning showed phlyctena at left kidney. She has not received western medical treatment so far. She got stomach and intestine sensitiveness and fever easily and had chronic astriction, erosion and desquamation of the lips, overmuch skin chromatosis at neck, face and forearm, and senile plaque. She still had agitation, bad sleep, dreaminess, listlessness, eye dryness, and chest pain.
Physical examination showed that rhagas and desquamation were found at lips, adnexal thickening and tenderness of sternal rib joint, fixed tenderness points at the connection of breastbone to costal margin of 6th to10th ribs (left) and 9th to 10th ribs (right). Abdomen was soft and swollen, hepatic region got percussion tenderness, and liver located 1.5cm down prime rib. Edema of lower extremities, finger indentation (+), lower extremities vena emergent, capillary vessel dilatation was at limited region beside left knee.
In the return visit after 4 copies of traditional Chinese medicine, liver deflated to be normal level. She herself thought to have gotten dull pain at abdomen, headache, cough, dark urine, and dryness heat after taking the Chinese medicine. Desquamation at lips, adnexal thickening and tenderness of sternal rib joint. After using the Chinese medicine one week, headache and dark urine disappeared. To go on taking the Chinese medicine, stomachache, paralysis at the limbs and trunk, overmuch phlegm, bad sleep, dreaminess and hypopiesia (80/50 mmHg) occurred reiteratively. But they all disappeared while the patient went on taking the Chinese medicine.
Observing with suspension of the drug after usage of 42 copies of the medicine, sneeze occurred during the suspension. Gentle fixed tenderness was still at breast joint of 9th left rib. Slight desquamation at lips, little phlegm, white face, no edema at lower limbs, no other abnormity. It was cured clinically. To observe with quit of the medicine.
|
||
| Case 2
Liang X (computer 2261), female, 42 years old. First visit at October 2000. She herself said that she had been sickly since childhood, with repeating skin pruritus and skin rash in the past years. Last November, she got erythema itch around the right eye socket, on the back and extremities. Biopsy at health center proved it to be cazenaves lupus. Blood and urine test showed no abnormity. There was no effect after repeating treatment of Chinese and western medicine and special treatment. Patient appeared listlessness, drowsiness, eye cloudiness (vitreous opacity at left eye), disturbance of menses, and vermeil abundant menses with little sludge. And she had chronic migrant skin rash and drastically skin pruritus.
Physical examination: Measles pimple could be found at the skin of top right internal canthus. At left back, palm-large ecchymosis and scratch mark appeared. Beat of pulse was 80 times per minute. Costal regions were malformed. Hepatic region got percussion tenderness and liver located 1.5 cm down prime rib. After taking 3 copies of the Chinese medicine, bilious headache broke out acutely, patient got aversion to wind and cold, pulse was 72 times per minute. Erythema was apparent on the face, and erythematous edema occurred at skin of right internal canthus, but liver located normally 1.5 cm top of prime rib.
When patient went on taking the Chinese medicine three copies, headache got relief. She herself thought to be skin pruritus. Patient got watery diarrhea, and the quantity was large. Another usage of three copies of the Chinese medicine stopped headache, alleviated skin pruritus. Accounting in her own words, she needed no western antipruritic or daub drug for exterior use. Erythema at right internal canthus retreated, and presented as brown pigmentation spot. Erythema at top right eyelid subsidized, attenuated and reduced apparently. After 9 copies of the Chinese medicine in all, physical examination showed that hepatic dullness area was still normal, and edema on the lower limbs disappeared.
When it was two weeks after beginning to take the Chinese medicine, erythema on the right eyelid subsidized apparently, and teeth prints in the tongue abated. Going on to take treatment with the Chinese medicine everyday till one month, patient seldom felt skin pruritus at down right eyelid, could go back to work, seldom felt headache, and got no hypersensitivity when contacting with abluent. Additionally, menses was vermeil and in normal quantity, with slight sludge.
Patient totally took 87 copies of the Chinese medicine, and that caused no discomfort, no skin rash, some listlessness, while stomach inhalement was ok. After clinic cure, we stopped Chinese medical treatment and switched to observation. |
Figure 5 and 6 below are the comparisons about the lip-mucosa pathological changes before and after treatment of Case 2>
Dated : 15th March 2001